10 Posture and Balance
Posture and Balance
“How one walks through the world,
the endless small adjustments of
balance, is affected by the shifting
weights of beautiful things.”
― Elaine Scarry

Posture
Posture is the position or attitude in which the body is held, such that individuals can have a supine posture, a sitting posture, and a standing posture. Posture has 3 functions. First, it functions to maintain alignment of the body’s segments in any position. Standing posture is often illustrated with a plumb line that runs from the top of the skull through the
ear, neck, shoulders, hips, knee and instep (Fig 10.1). The second function of posture is to anticipate change, which allows the body to engage in voluntary, goal-directed movements. For example, when stepping or reaching, the body makes postural adjustments before, during and after a movement. Third, posture is reactive to unexpected perturbations.
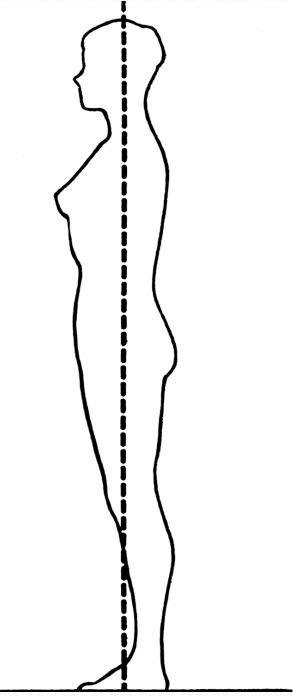
Figure 10.1 Standing Posture
Balance/Postural Control
Postural control is determined and maintained through coordination of the central nervous system (CNS), the sensory system and the musculoskeletal system. Together, these systems produce muscular strategies to regulate the relationship between the center of mass (COM) and the base of support (BOS) (Maki & McIllroy, 1996). In other words, postural control is the act of maintaining, achieving, or restoring a state of balance during any posture or activity (Pollock, Durward, Rowe, & Paul, 2000).
There are four types of postural control: static, reactive, anticipatory, and adaptive. Static postural control ensures stability by maintaining the body’s COM within its BOS. Although balance in quiet standing is considered static, subtle movements are occurring during quiet standing.
Reactive postural control governs the unexpected movement of the COM within or outside the BOS. An example of reactive postural control is an unexpected perturbation on a force platform. The movement of the platform shifts the person’s COM resulting in the need for a postural adjustment.
Various balance responses are possible given the speed of the displacement and whether the displacement results in the COM exceeding the BOS. Righting or equilibrium reactions are produced in response to weight shifts within the BOS. When the COM moves out of the BOS, as in a slip or fall, additional automatic postural responses occur.
Postural adjustments made before a movement are classified as anticipatory. Typically, postural adjustments occur before reaching, lifting, and stepping. Anticipatory postural adjustments require that the nervous system feed information forward to postural muscles to prepare for the movement to follow. Experience is important in acquiring effective and efficient anticipatory postural control.
Lastly, adaptive postural control is demonstrated when a motor response is modified because of a change in environmental conditions or task demands. For example, most individuals change their speed and step width when walking on slippery surfaces, such as ice. Aspects of cognition, such as attention, motivation, and intention, can influence anticipatory and adaptive postural control. When attention is directed away from the balance task, it may be more difficult to adapt.
Balance is the term many clinical specialties use to describe postural control. Figure 10.2 illustrates the physiologic components known to interact during the process of achieving and maintaining balance/postural control.
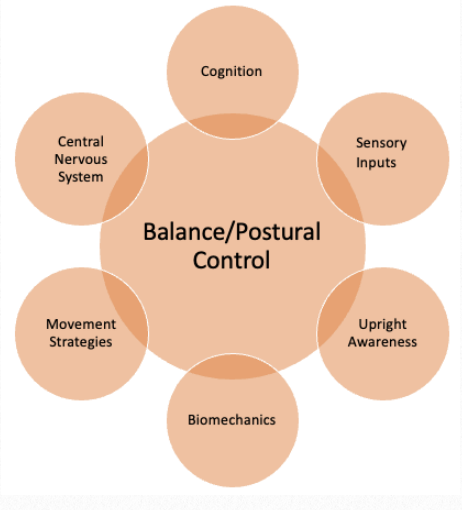
Figure 10.2 Components of Balance/Postural Control
The three sensory systems that are mainly involved in balance or postural control are the somatosensory (proprioception), the visual and the vestibular systems. In any given situation, the CNS is responsible for prioritizing the information from one system to another in order to maintain balance in different conditions.
The ability to choose and relay the appropriate sensory input for each condition is sometimes referred to as sensory re-weighting. For example, when a person is standing on an unstable surface, the CNS increases sensory weighting to vestibular and visual information and decreases the dependence on surface somatosensory inputs. Likewise, when a person is in the dark, balance control depends primarily on somatosensory and vestibular feedback (de Oliveira, de Medeiros, Frota, Greteers, Conforto, 2008).
The visual system is important for determining orientation and alignment relative to objects and features of the environment. When light strikes the sensory receptors in the retina, it sends impulses to the brain that provide the visual cues necessary to oriented oneself to the surrounding environment.
The somatosensory system combines the sensory inputs of touch and proprioception to provide a sense of body schema and an awareness of the relationship between one’s body and the outside world. Information from the sensory receptors found in skin, muscles and joints, such as the mechanoreceptors (e.g. Pacinian and Meissner corpuscles, Merkle disks, Ruffini endings) and the proprioceptors (e.g. muscle spindle and Golgi tendon organ) help detect the position of body parts in space, and information about joint movement and position.
The vestibular system is part of the inner ear and is responsible for monitoring head position. It also contributes to a sense of equilibrium, which combines balance and orientation in space. Information received from eye movement, as well as head movement, are coordinated through the vestibular system. The vestibular apparatus in the inner ear, sometimes known as the labyrinth is comprised of the cochlea, semicircular canals, utricle and saccule. They function to detect the position and movement of the head and aid in maintaining equilibrium in different contexts.
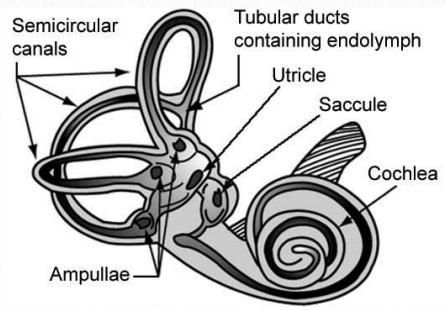
Figure 10.3 Vestibular System
Information from the eyes, somatosensory receptors and the vestibular system is sent to the brainstem. Here the input is sorted and integrated with information from the cerebellum and the cerebral cortex. The cerebellum provides information about automatic movements that have been learned through repeated exposure and demands. The cerebral cortex contributes previously learned information such as “ice surfaces are slippery” which then activates a different walking pattern to navigate safely.
Prenatal
The sense of touch, as well as the vestibular and visual senses begin to develop during the prenatal period. The vestibular apparatus can be observed in the primitive ear as early as the fourth week of gestation. The ability to respond to touch around the mouth appears at approximately eight weeks (Jeffery & Spoor, 2004).
By week ten the semicircular canals, utricle and saccule are completely formed. At about the same time, the developing fetus has been observed to respond to proprioceptive inputs of tapping, stretching and changes in amniotic fluid pressure.
At approximately 12 weeks, there is further advancement of the somatosensory and vestibular systems. Muscle spindles begin to differentiate, and neural connections between the labyrinths and the oculomotor nuclei in the brainstem begin to develop. Golgi tendon organs, Pacinian corpuscles, and sensory nerve endings carrying pain are typically found by 20 weeks. However, the pathway from the spinal cord to the cortex is incomplete at this time and so the fetus does not feel pain. This pathway connects to the thalamus at approximately 24-26 weeks, making cortical perception of pain possible, although complete myelination of the nocioceptive system does not occur until 37 weeks of gestation.
Infancy and Early Childhood
Complete maturation of sensory pathways occur after birth as evidenced by increases in nerve conduction time, axon branching and increased synaptic efficacy. Changes also occur as a result of needing to function outside of the mother’s womb.
In neonates, somatosensory information is initially used to help locate food and although touch and pain are not completely differentiated at birth, this happens very dramatically over the first four days of life. By one month, an infant can sense the difference between pacifier shapes and by seven-nine months moves from reflexive responses to touch to being able to localize touch. This ability continues to become refined until almost two years of age (Rigato, et al, 2014).
Achieving and maintaining an upright posture is dependent on an infant’s ability to interpret and respond to information about body sway, which comes from vestibular, visual and proprioceptive in put. The first evidence of this integration is the vestibulo-ocular reflex (VOR) in which activation of the vestibular system causes eye movement. This reflex functions to stabilize images on the retinas during head movement by producing eye movements toward the opposite direction. Maturation of the vestibular system contributes to postural control
and general motor development through its contribution to developmental reflexes. Examples of reflexes related to postural control include head righting, equilibrium reactions and protective reactions.

Figure 10.4 Upright Sitting with Vision
Righting means to bring the body into “normal” alignment. The essence of righting is movement from one stable posture to another. Righting reactions begin at birth and exhibit peak occurrence at 10-12 months. These reactions can be elicited by any number of sensory stimuli: vestibular, proprioceptive, visual, or tactile. Another type of righting response produces rotation. An example is rolling, a movement in which body segments maintain a functional alignment. Mature neck- and body-righting allow for the developmental progression of log
rolling to segmental rolling in infants.
Righting reactions become incorporated into the more sophisticated equilibrium reactions, which involve a total body response to a slow shift of the center of gravity outside the body’s base of support (BOS). Equilibrium reactions begin to appear at 6 months of age in the prone position, even as the infant is experiencing supported sitting. The remaining equilibrium reactions appear in an orderly sequence: prone, supine, sitting, quadruped, and standing. The maturation of the reactions in these postures lags behind the attainment of movement in
the next higher developmental posture. For example, equilibrium reactions mature in the sitting position when the child is creeping and mature in the quadruped position when the child is walking.
Protective reaction is an extremity response to a quick displacement of the center of gravity out the BOS. The earliest protective reactions is observed at 4 months and is the downward or extension response when the infant is quickly moved to a supportive surface. Upper extremity protective reactions begin in sitting at 6 months and are observed when the infant begins to tip over.
Sometimes called protective extension, this reflex tends to develop sequentially, first forward, followed by sideways and then, backward. Protective reactions are generally completely developed by ten months of age. These reactions persist and become a backup system if we fail to regain our balance by using equilibrium reactions. Unfortunately, use of
these automatic responses can result in unintentional injury, as when a young child sustains a greenstick fracture of the forearm or an older adult sustains a Colles fracture from falling onto an outstretched arm.
Prior to upright sitting, it is obvious that postural development proceeds from head control to trunk control, with many infants able to assume a prone on elbows posture as young as three weeks. Weight bearing in this posture is important for developing proximal shoulder girdle stabilization. The prone progression proceeds from prone on elbows to prone on extended arms and then to quadruped.

Figure 10.5 Early Standing Posture
With achievement of upright stance, erect posture is precarious. Because the infant’s newly erect center of gravity is relatively high (T12 compared with L5- S1 in an adult), and forward (due to a proportionally larger liver) an infant’s base of support is quite wide in standing. For the upper trunk to achieve a vertical position, lumbar lordosis is increased, and the arms
are brought into a high guard position. Initially, infants and toddlers also tend to have flat feet and genu varus, but this is seen to resolve as the child spends more time in weight bearing. Weight bearing also precipitates a diminishing fat pad in the foot and development of the longitudinal arch.
Childhood and Adolescence
During childhood, integration of sensation and movement becomes more sophisticated. Perceptual processes, in which children can attend to multiple stimuli and plan a motor response, are also refined. Touch and proprioception continue to develop in childhood so that by the age of four, most children have two-point discrimination and five year olds can
identify familiar objects by touch. Movement during this time allows children to use proprioceptive information to advance self-recognition. As Thelen (1995) suggested, individuals perceive in order to move and move in order to perceive.
Kinesthetic acuity is the ability to proprioceptively discriminate differences in location, distance, weight, force, speed, and acceleration of movement and improves with age. Researchers have reported that kinesthetic acuity improves in children from age five through twelve and sometimes beyond (Livesey, 2002).
Memory for movement is known as kinesthetic memory. Examples of movement tasks performed from memory are activities such as a dance routine or something as basic as skipping, which is a sequence of step-hopping. Adult levels of kinesthetic memory are usually achieved until age 12.

Figure 10.6 Girls Performing a Venezuelan Dance
Directionality, which is the motor expression of laterality and spatial awareness, also continues to develop until approximately 12 years of age. Given the development of kinesthetic acuity and memory, along with the refinement of directionality that occurs during the pre-teen years, it’s no wonder that teaching young children dance choreography or other motor tasks that require multiple, sequential steps can be very challenging.
Adults and Older Adulthood
Integration of the different types of sensory information that influence posture and balance is maintained through middle age. Musculoskeletal changes along with sensory systems changes account for the alteration of posture observed in older adults. During this time however, the decline in these systems do not directly correlated with a decline in function, nor do the degree of changes appear to universal.
Typical postural changes of older adulthood can be seen in Figure 10.7. To a large extend, the more flexed posture is due to a decline in strength and flexibility. However, the most commonly observed older adult posture may also reflect a sub-conscious desire to alter ones center of mass and base of support in order to achieve greater stability.
Given the interactions required for postural control and balance, it is relevant to note that many older adults will demonstrate a decreased ability to detect touch, vibration, proprioception, This is in part due to changes in connective tissue as well reductions in the number of receptors that are sensitive to pressure and light tough. One of the most common sensory losses noted in older adults is the loss of vibratory sensation, due to a decline and alterations of the Meissner’s and Pacinian corpuscles. Changes is vibratory sensation can occur as early
as 50 years of age and may be related to the age related decline in balance seen in many older adults. In addition, joint position sense declines with age especially in the lower extremities, with the distal toes and ankles more affected than the knees and hips.

10.7 Postural Changes Often Seen with Aging
These observations likely contribute to changes in balance reactions as people age. Older adults respond differently to external perturbations than younger adults because they tend to initiate their reactions at the hips rather than at the feet or ankles. Furthermore, older adults tend to take steps to regain their balance and do so earlier and more frequently than younger people. Stepping reactions, in particular lateral stepping and crossover steps are associated with a history of falling.
Presbystasis is the age-related decline in equilibrium or dynamic balance seen when no pathology is observed. This may be related to observations that older adults have a reduced number of hair cells in the saccule, utricle and semi-circular canals compared to younger people. In addition, neural changes in the vestibular nerve are evident in older adults, with a 40% decline in the number of myelinated vestibular nerve fibers by 75 years of age. Fortunately the nervous system is most often able to compensate for age-related deterioration of the
vestibular system. However, dizziness and vestibular dysfunction such as vertigo may manifest when the nervous system is no longer able to compensate. Given the changes that occur in the multiple sensory systems that contribute to balance it’s no surprise that older adults present with an increased risk of falling. Unfortunately, one quarter of Americans over the age of 65 fall every year, with falls being the leading cause of fatal injury in older adults.
Final Thoughts
Posture and balance rely on the interactions of the central nervous system, the sensory systems and the musculoskeletal system. Despite development and decline at varying rates, these systems continue to integrate important information and play a critical role in organizing responses to external disturbances of posture and balance over a life time.
References
Jeffery, N., & Spoor, F. (2004). Prenatal growth and development of the modern human labyrinth. Journal of Anatomy, 204(2), 71-92.
Livesey, D. J. (2002). Age differences in the relationship between visual movement imagery and performance on kines8 10.7 Postural Changes Often Seen with Aging thetic acuity tests. Developmental Psychology, 38(2), 279– 287. https://doi.org/10.1037/0012-1649.38.2.279
Maki, B.E., & McIlroy, W.E. (1996).Postural control in the older adult. Clinics in Geriatric Medicine, 12(4), 635-58.
Pollock, A.S., Durward, B.R., Rowe, P.J., & Paul, J.P. (2000). What is balance? Clinical Rehabilitation, 14(4), 402-406.
Rigato, S., Ali, J.B., van Velzen, J., Bremner, A.J. (2014). The neural basis of somatosensory remapping develops in human infancy. Current Biology, 24(11), 1222-1226.
Thelen, E. (1995). Motor development: a new synthesis, American Psychologist, 50, 79-95.
Images
Title page. Balance. Photo by Szabolcs Takacs. Retrieved from https://www.istockphoto.com/photo/two-children-onrails-gm525352083-51913588. Licensed on 2/23/22.
Figure 10.1 Standing Posture. PostureFoundationGarments04fig2.png|PostureFoundationGarments04fig2. Retrieved from https://commons.wikimedia.org/w/index.php?
search=standing+posture&title=Special:MediaSearch&go=Go&type=image
Figure 10.2 Components of Balance/Postural Control (adapted from de Oliveira, et al., 2008). http://www.rehab.research.va.gov/jour/08/45/8/barros-de-oliveira.html
Figure 10.3 The Vestibular System. Image from NASA. Retrieved from https://upload.wikimedia.org/wikipedia/commons/c/c9/Vestibular_organs-_canals%2C_otolith%2C_-
cochlea.jpg
Figure 10.4 Upright Sitting With Vision. Retrieved from https://www.usda.gov/media/blog/2014/05/06/developingnational-dietary-guidance-birth-24-months-age-group
Figure 10.5 Early Standing Posture. Photo by Sean Dreilinger. Retrieved from https://wordpress.org/openverse/image/3a8ed533-4206-4de2-8de6-2b600697c2cc
Figure 10.6 Girls Performing a Venezuelan Dance. Photo by Ricardoricardo618. https://upload.wikimedia.org/wikipedia/commons/b/b6/Children_performing_artistic_dance_-_Danza_art%C3%ADstica_ejecutada_por_ni%C3%B1os.JPG
Figure 10.7 Postural Changes Often Seen with Aging. Image credit: urfinguss. Licensed Feb 25, 2022.

