3 Development & Changes of the Cardiovascular & Pulmonary Systems
“We humans can never claim to do
nothing, we breath, we pulse, we regenerate.” ― Suzanne Weyn

Cardiovascular system
The cardiovascular system is comprised of the heart and blood vessels, including arteries, veins, and capillaries. The heart is responsible for pumping blood throughout the body via the arteries and smaller capillaries. From the heart, blood carries nutrients and oxygen to the cells which is exchanged between the capillaries and the tissues. Then, the veins allow blood to return to the heart, transporting metabolic waste products along the way.
Heart rate refers to the number of times the heart beats per minute, whereas stroke volume is the amount of blood pumped with each beat. When the heart rate is multiplied by the stroke volume, an individual’s cardiac output can be determined. This is the amount of blood pumped by the heart in one minute.
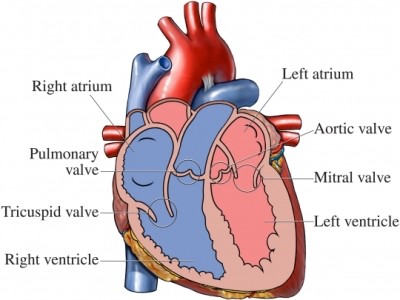
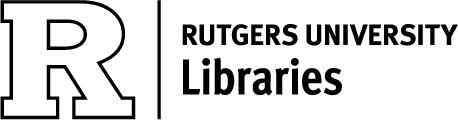
Figure 3.1 Chambers and Valves of the Heart
The heart has four chambers, two atria and two ventricles (Figure 3.1) The atrium on the right gets blood from the body that’s low in oxygen and pumps it to the right ventricle via the tricuspid valve. The right ventricle then pumps blood to the lungs through the pulmonary valve to pick up oxygen. The oxygen rich blood is then sent to the left atrium which is pumped to the left ventricle via the mitral valve. The oxygen rich blood gets pumped out of the left ventricle to the rest of the body by way of the aortic valve (Aaronson, et al, 2020).
Prenatal Period
The cardiovascular system is the earliest system to function in the developing embryo. By the 3rd week of gestational age, blood has begun to circulate and a primitive heart tube is formed. This tube establishes links with its blood vessels and with the placenta so that circulation can be established between the mother and the embryo.
Vascular development begins with the differentiation of mesodermal cells into vessels. The formation of blood vessels is called angiogenesis, which can occur during the embryonic period as well as throughout the lifespan. By the 7th week, the heart tube has developed into a four-chambered vessel. The fetal circulatory system uses two shunts in order to bypass the lungs and the liver, organs that are not fully developed in the womb. The foramen ovale is the shunt that moves blood from the right atrium to the left atrium. The ductus arterioles is the shunt that moves blood from the pulmonary artery to the aorta. The fetus receives all of its oxygen and nutrition from the mother’s blood which is transferred across the placenta via the umbilical cord. Waste product and carbon dioxide from the fetus are also sent through the umbilical cord and placenta. This allows for elimination via the mother’s circulation.
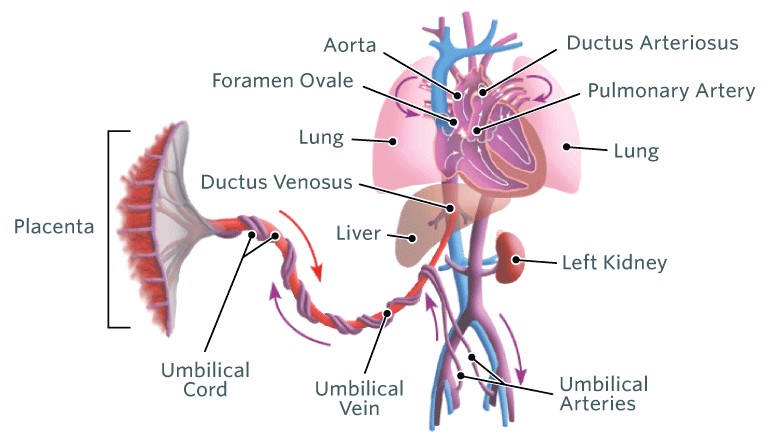
Figure 3.2 Fetal Circulation
At birth, the umbilical cord is clamped, thereby cutting off oxygen and nutrients from the mother. With the infant’s first breaths the lungs expand and the alveoli in the lungs are cleared of fluid. This results in a significant reduction in pulmonary pressure, which reduces the need for the ductus arterioles to shunt blood and gives rise to the closure of the shunt. These changes increase the pressure in the left atrium, which decrease pressure in the right atrium and in turn, stimulate the foramen oval to close. The closure of these ducts signal the transition from fetal circulation to newborn circulation (Mathew, et al. 2021).
Infancy and Childhood
Through infancy and childhood, the rate of development of the cardiovascular system is similar to the increase in body size, although during the first year of life, the heart grows a bit more slowly than the rest of the body. At 12 months of age, many infants have tripled their weight, whereas heart size has doubled. During this time the vascularization of the heart muscle increases and the left ventricular wall becomes thicker, due to the work of pumping blood throughout a growing body (Cech & Martin, 2012).
Figure 3.3 Heart Rate of Infants through Early
Adolescence
Arteries and veins also change in size with thickness of the vessel wall increasing in sync with increased functional demands. It is important to realize infants and children have very different mean heart rate and stroke volume values than adults. This is because stroke volume is related to heart size. With a small heart, less blood can be pumped with each beat. To compensate for this, children demonstrate higher heart rates than adults. However, as the heart gets stronger, and infants develop into children, heart rate drops. When awake, infants
have heart rates of 100-205 beats/minute, whereas the normal heart rate of an 11 year olds ranges between 75-118 beats/minute (Fleming, et al, 2011).

Figure 3.4 Blood Pressure of Infants through Early Adolescence
Blood pressure changes also occur during the development of infants and children. Unlike heart rate, though, blood pressure increases. This change is associated with ongoing development of the autonomic nervous system, peripheral vascular resistance and body mass (Saikia & Mahanta, 2019).
Adolescence
During infancy and childhood, changes of the cardiovascular system are largely driven by increases in body height and weight, which are similar between boys and girls. During the adolescent period however, sex differences become apparent. While the left ventricular mass increases with body mass equally between boys and girls for ages 9-12 years, in adolescence, the left ventricular mass of males becomes greater than females. Regardless of sex however, those who participate in endurance activities and sports will have greater ventricular mass
than those who do not participate in these types of activities.
During adolescence the amount of heart muscle increases which results in a decrease in heart rate and an increase in blood pressure. In females, blood pressure increases during the prepubertal growth spurt, then levels off. In males, blood pressure gradually increases with lean body mass through eighteen years of age. By the end of adolescence, the systolic blood pressure of males becomes slightly higher that those of females, however, no differences are observed with diastolic blood pressure. Sex differences are also noted with heart rate such that basal heart rate is 3-5 beats faster in females than in males.

Figure 3.5 Aerobic Activity
Peak height velocity (PHV) is the period of time during which maximum rate of growth occurs. In the year before PHV, stroke volume changes appear to be related to an increase in the arterial-venous oxygen difference. This difference is indicative of how much oxygen is removed from the blood through the capillaries. Thus, an increase in arterial-venous oxygen means that more oxygen is being extracted by the tissues, which is likely due to age-related changes in muscle mass, muscle enzyme profusion, and the ratio of capillaries to muscle fiber. In the year after PHV, an increase in stroke volume is noted. This may be due to an enhanced cardiac preload condition with an increased venous return. Preload is related to chamber volume and the sarcomere length of the cardiac muscle fibers just prior to contraction (Cech & Martin, 2012).
Adulthood and Aging
Over time there are changes in the cardiovascular system which result in a general functional decline. However, normal aging changes that occur in cardiovascular physiology must be differentiated from pathological changes, including conditions such coronary heart disease and atherosclerosis.
Many changes in the cardiovascular system are associated with a decrease in elasticity and an increase in stiffness of the arterial system. These alterations in connective tissue can have dramatic effects on the aorta and left ventricle. As the aorta becomes less compliant, there is increased resistance to ejection of blood from the left ventricle, which results in left ventricular hypertrophy and slowing of ventricular relaxation (Cheitlin, 2003).
The negative effect aging has on muscle, including heart muscle, in combination with the heart needing to overcome the increased stiffness of the vessels and ventricular wall, is associated with decreases in both maximal heart rate (MHR) and stroke volume (SV). As the product of MHR and SV, cardiac output also decreases with age.
In the endocardium itself, thickened areas of elastin and collagen fibers are common especially in the atria. In addition, increased fat is found within the epicardium. With aging, changes are also seen in the heart valves and conduction system. Valves become thickened and calcified which can impair their ability to completely close which gives rise to increased incidence of heart murmur in older adults. Collagen and fat are also found in the left bundle branches and by the age of fifty, the number of pacemaker cells in the sino-atrial node has already
begun to decrease. Other changes in the conduction system include cellular loss at the atrioventricular node, decreased responsiveness to adrenergic receptor stimulation and decreased reactivity to baroreceptors and chemoreceptors. These alterations may contribute to common electrocardiogram (ECG) findings in older adults such as premature ventricular contractions, QRS wave shifts to the left, and ST segment depression.
Pulmonary System
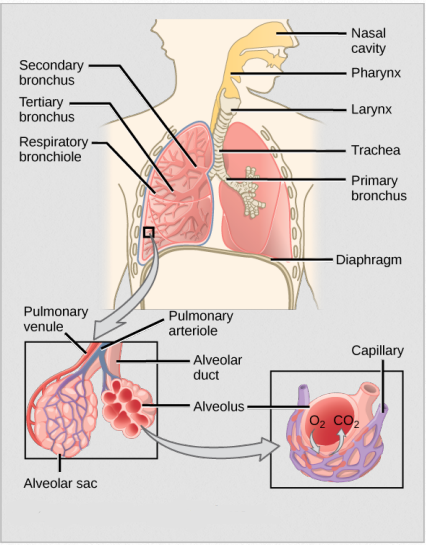
Figure 3.6 Pulmonary System
The pulmonary system is responsible for taking in oxygen and expelling carbon dioxide. This life-sustaining process begins with oxygen entering the body through the nose or mouth and passing through the sinuses which help regulate the temperature and humidity of the air. Air passes through the trachea, which branches into two bronchi. The bronchial tubes are lined with tiny hairs called cilia, which act to filter the inhaled air and carry mucus up and out of the body.
The bronchial tubes lead to the lobes of the lungs and divide into further branches called the bronchioles. Within the lobes of the lung, bronchioles terminate in spongy sacs called alveoli. The alveoli have extremely thin walls, comprised of a single layer of epithelial cells and tiny pulmonary capillaries. Gas exchange occurs at the level of the alveoli and capillaries.
The diaphragm, a dome-shaped muscle at the bottom of the lungs, is the primary muscle of respiration. During inspiration, the intercostal muscles elevate the rib cage and the diaphragm flattens, increasing negative pressure in the expanded thoracic cavity. As atmospheric air rushes in, the lungs expand and the bronchi increase in diameter. Exhalation occurs passively, with muscle relaxation and elastic recoil of the chest wall.
The transport of inspiratory and expiratory gases is strongly influenced by the ability of the musculoskeletal components of the pulmonary system to act as a pump. This requires appropriate levels of compliance and resistance of the chest wall and lungs. Flexibility of the connective tissue and joints of the thoracic cavity allow for optimal expansion. Resistance and elasticity of the pulmonary tissues must be overcome by contraction of all the respiratory muscles. Resistance of the conducting airways also affects the work of the pulmonary system.
The maximum amount of air that can be contained in the lungs is known as the total lung capacity (TLC), and the amount of air that is moved during resting inhalation and exhalation is called the tidal volume (TV). The extra air that can be taken in with a deep inhalation is called the inspiratory reserve volume (IRV), whereas the additional air that can be pushed out of the lungs with a forceful exhalation is the expiatory reserve volume (ERV). The TV, combined with the IRV and the ERV is known as the vital capacity (VC) and the amount of air that’s left in the lungs after exhalation is the residual volume (RV). Forded expiratory volume (FEV1) is the maximal amount of air that can be forcefully exhaled in one second and is influenced by aforementioned values. FEV1 is one of the most common indices used to assess airway obstruction.
Prenatal
The pulmonary system of the embryo first appears during the 4th week of gestation with formation of the bronchial buds. This is followed by development of at least two respiratory bronchioles at approximately twelve weeks. Development of the pulmonary tree continues including terminal bronchioles and primitive alveoli. The structure of the primitive alveoli becomes more complex throughout prenatal development and the number of alveoli continue to increase even after birth, until approximately eight years of age (Rehman & Bacha, 2021).
At about twenty-four weeks of gestation, Type II epithelial cells within the primitive alveoli begin to produce a substance called surfactant. Surfactant is a complex mixture of lipids, proteins and carbohydrates that acts to decrease the surface tension at the air-liquid interface of the alveoli. This allows for sufficient vascularization of the terminal sacs, so
that maximum lung expansion can occur after birth. By weeks 24-26, the fetus should have enough surfactant and vascularization to survive if born prematurely.
In utero, the lungs are not responsible for gas exchange. Instead, the mother provides blood and oxygen to the fetus via the umbilical artery. Fetal lung tissue actually secrets a liquid that is swallowed or added to the amniotic fluid. Shortly before birth, the fluid production slows so that the lungs are only 50% filled at the time of deliver.
Infancy and Childhood
Immediately after birth, the fluid in the lungs must be removed so that the lungs can fully inflate. Much of the fluid is pushed out through the nose and mouth as a result of pressure on the thorax during the birth process. The remaining fluid is drained by the pulmonary vasculature and lymphatic system. With inspiration, alveolar expansion occurs, delivering oxygenated air to the alveoli.
As the bronchioles and alveoli continue to proliferate and develop during infancy and childhood, an increase in the gas exchange capacity of the lungs is realized. This does not suggest however, that children have the same capacity as adults. Smooth muscle in the walls of the bronchioles do not develop until 3-4 years of age, which means that they are more susceptible to collapse at a young age. In addition, the elastic tissue in the alveoli is incomplete although it continues to develop through adolescence. This in effect, limits lung compliance and distensibility and makes it harder for infants and toddlers to fully inflate their lungs and maintain lung volume.
Structurally, it should be noted that the conducting and respiratory airways are small in children, increasing in length and diameter until growth of the thoracic cavity is complete. The impact of small airways is that 1) the work of breathing is increased due to vessel resistance, and 2) they are easily obstructed by foreign objects. Another structural limitation of the pulmonary system in children is decreased collateral circulation. The combination of small airway size, impaired distensibility and little collateral ventilation mechanisms puts children at
higher risk for respiratory infections and atelectasis.
Lung volume and vital capacity will increase during childhood proportionally with increases in body size and the development of more alveoli. During the first year, infants have little pulmonary reserve and must increase their respiratory rate to meet demands for increased oxygen. Inspiratory and expiratory reserve volumes sufficient to meet increased needs are evident at about one year of age (Saikia & Mahanta, 2019).
Adolescence
During the adolescent growth spurt, there are increases in the size of proximal airways, vasculature, and the lungs themselves. The alveoli also get larger and develop a greater amount of elastin. At the same time, the capillaries in the alveolar region are also getting larger, which allows for enhanced gas exchange. Growth and development of the pulmonary system is essentially complete by 18-20 years of age (Fleming, et al 2011).
Adulthood and Aging
Most indicators of pulmonary function have pretty much reached their maximum level between 20-25 years of age. After that, there are declines in the functioning of the pulmonary system consistent with normal aging. To a great extent, the declines are due to changes in connective tissue. First, there are alterations in the chest wall structure. The thorax becomes stiffer and shorter over time with decreased mobility of the joints that allow rib rotation. A decrease in respiratory muscle strength is also observed during the aging process. The combination of weakness and stiffness results in a decrease of chest wall expansion and an increase in the effort to breathe (Sharma & Goodwin, 2006).
Connective tissue changes, specifically collagen and elastin result in decreased recoil of the lungs and alveoli, especially at high lung volumes. As elastic recoil of the lungs becomes limited, residual volume increases and vital capacity is reduced. Loss of alveolar recoil, along with a decline in alveolar surface area also contribute to a higher residual volume and account for a ventilation-perfusion mismatch, which has a negative effect on gas exchange. The decreased elasticity and surface area of the alveoli make them vulnerable to collapse on expiration. In addition, these changes are associated with a decrease in arterial PO2, which reflects a decline in the ability to pull oxygen into the blood from the air.
Cardiorespiratory Fitness
Anatomical and physiological differences of the cardiovascular and pulmonary systems are observed at each stage of development. Through childhood, most changes are related to increases in height and weight. During adolescence, sex differences are observed. In adulthood, normal aging changes are associated with declines in function, however, lifestyle habits such as proper nutrition and exercise can have positive effects on both systems. Smoking on the other hand, has a negative effect on both the cardiovascular and pulmonary systems.
Fitness, which is considered to be a measure of a person’s functional ability and health, is impacted by changes in cardiac factors and the diminished ability of peripheral tissues to extract oxygen. As early as age 30, the average person is already beginning to see declines in peak VO2. Initially, the decline is approximately 5% per decade, but the rate of decline increases after 45 years of age, so that by age 70, there is a 20% decline per decade. Cardiorespiratory fitness of both sexes decreases to approximately 65% of peak aerobic capacity. Individuals who have maintained high levels of physical activity throughout their life, have higher levels of peak oxygen uptake as they become older adults and maintain higher levels of cardiorespiratory fitness than their peers. Nevertheless, these fit individuals will still experience a decrease in cardiorespiratory fitness with increasing age.
Changes in the functional lung volumes and decreased efficiency of the respiratory muscles reduce an older person’s ability to increase tidal volume and minute ventilation in response to exercise. However, these changes typically do not negatively effect an older person’s capacity at rest and are minimized in healthy, active, non-smoking adults especially those who are engaged in endurance training (Jackson, et al, 2009).

Image 3.7 Endurance Activity
Final Thoughts
The cardiovascular and pulmonary systems work closely together to support the basic physiologic processes of life and so, changes in these systems over time will alter an individual’s functional ability. It is important to consider cardiovascular and pulmonary development and function across the lifespan when working with patients and clients during the rehabilitation process and when advising them about how to minimize the effects of aging.
Regardless of age, regular physical activity at an appropriate level of intensity, will help to maintain maximal efficiency of both the cardiovascular and pulmonary systems.
References
Aaronson, P.I., Ward, P.T., Connolly, M.J. The Cardiovascular System at a Glance, 5th ed. Hoboken, NJ: Wiley-Blackwell, 2020.
Cech, D. J. & Martin, S. T. Cardiovascular and Pulmonary System Changes in Functional Movement Development Across the Life Span, 3rd ed. St. Louis, MO: Elsevier, 2012.
Cheitlin, M. D. (2003). Cardiovascular Physiology -Changes with Aging. American Journal of Geriatric Cardiology, 12(1), 9-13.
Fleming S, Thompson M, Stevens R, Heneghan C, Pluddemann A, Maconochie I, Tarassenko L, Mant D. (2011). Normal ranges of heart rate and respiratory rate in children from birth to 18 years: a systematic review of observational studies. The Lancet, 377(9770),1011-1018.
Jackson, A. S., Sui, X., Hébert, J. R., Church, T. S., & Blair, S. N. (2009). Role of lifestyle and aging on the longitudinal change in cardiorespiratory fitness. Archives of Internal Medicine, 169(19), 1781–1787. https://doi.org/10.1001/archinternmed.2009.312
Mathew P, Bordoni B. Embryology, Heart. [Updated 2021 Aug 11]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https:// www.ncbi.nlm.nih.gov/books/NBK537313/
Rehman S, Bacha D. Embryology, Pulmonary. [Updated 2021 Aug 11]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https:// www.ncbi.nlm.nih.gov/books/NBK544372/
Saikia, D., & Mahanta, B. (2019). Cardiovascular and respiratory physiology in children. Indian Journal of Anaesthesia, 63(9), 690–697. https://doi.org/10.4103/ija.IJA_490_19
Sharma, G., & Goodwin, J. (2006). Effect of aging on respiratory system physiology and immunology. Clinical Interventions in Aging, 1(3), 253–260. https://doi.org/10.2147/
ciia.2006.1.3.253
Images
Title page. Cardiovascular System. [Image File]. Retrieved from http://www.fda.gov/ucm/groups/fdagov-public/documents/image/ucm463430.jpg
Figure 3.1 Chambers and Valves of the Heart. [Image File]. Retrieved from http://images.lifescript.com/images/ebsco/images/si55551150.jpg
Figure 3.2 Fetal Circulation. [Image File]. Retrieved from http://www.chop.edu/sites/default/files/fetal-circulation-illustration-canonical-16×9.png
Figure 3.3 Heart Rate of Infants through Early Adolescence. [Image File]. Retrieved from http://www.pedscases.com/pediatric-vital-signs-reference-chart
Figure 3.4 Blood Pressure of Infants through Early Adolescence. [Image File]. Retrieved from http://www.pedscases.-com/pediatric-vital-signs-reference-chart
Figure 3.5 Aerobic Activity. [Image File]. Retrieved from https://www.runnersworld.co.uk/health/8-minutes-of-running-a-day-can-boost-health-in-teenagers Section Title Image, Pulmonary System. [Image File] Retrieved from https://pixabay.com/en/upper-body-lung-copddesease-944557
Figure 3.6 Pulmonary System. [Image File]. Retrieved from https://openstax.org/books/concepts-biology/pages/16-3-circulatory-and-respiratory-systems
Figure 3.7 Endurance Activity. [Image File]. Retrieved from https://www.nia.nih.gov/news/exercise-induced-proteinmay-reverse-age-related-cognitive-declin