7 Development & Changes of the Endocrine System
Development & Changes of
the Endocrine System
“Hormones get no respect. We think of
them as the elusive chemicals that make
us a bit moody, but these magical little
molecules do so much more.”
-Susannah Cahalan

Endocrine System
The endocrine system is a network of glands and organs that affect nearly every physiological system and cell in the body. It produces hormones that regulate among other things metabolism, blood pressure, body temperature, blood glucose levels, growth and development, sexual function including reproduction, sleep, stress, and mood. Three glands that are located in the brain are the hypothalamus, pituitary and pineal gland. The hypothalamus works to maintain homeostasis by responding to stimuli and signals from the internal and external
environments. It responds to physiologic and psychologic stress and works to adapt and restore balance and optimal function. The hypothalamus provides the primary connection with the nervous system and is considered to be the control center because it signals the pituitary when to start and stopmaking hormones (Hiller-Sturmhöfel & Bartke, 1998).
Thyrotropin-releasing hormone (TRH), gonadotropin-releasing hormone (GnRH), growth hormone-releasing hormone (GHRH), corticotropin-releasing hormone (CRH), somatostatin, and dopamine are all secreted by the hypothalamus and travel to the anterior lobe of the pituitary where they exert their effects. The hypothalamus also synthesizes two hormones, vasopressin and oxytocin, which travel in the neurons themselves to the posterior lobe of the pituitary.

Figure 7.1 Hormones of the Hypothalamus, Thyroid, Pituitary and Pineal Gland
The pituitary has two lobes and is considered the master gland because the hormones it produces affects the functioning of many other glands and the release of their hormones. The anterior lobe secretes thyroid stimulating hormone (TSH) and prolactin (in females) which is stimulated by TRH. TSH is inhibited by somatostatin whereas prolactin is repressed by estrogens and dopamine. The anterior lobe of the pituitary also releases follicle-stimulating hormone (FSH) and luteinizing hormone (LH), both triggered by GnRH, which arrives from the hypothalamus. Human growth hormone (GH) is released by the anterior lobe of the pituitary in response to GHRH and affects most organ systems, whereas the adrenocorticotropic hormone (ACTH) is produced in response to CRH and acts on cells primarily in the adrenal cortex. The pituitary’s posterior lobe is responsible for releasing vasopressin and oxytocin into circulation, hormones that are synthesized in the hypothalamus.
The smallest of the endocrine glands located in the brain is the pineal gland, which produces melatonin, a derivative of the amino acid tryptophan. Synthesis and release of melatonin is stimulated by darkness and inhibited by light.
The thyroid and parathyroid glands are in the neck, with the parathyroids located behind the thyroid (Figure 7.2). The thyroid secretes triiodothyronine (T3) and thyroxine (T4) hormones that are derivatives of the amino acid tyrosine, along with calcitonin, a hormone that’s released in response to an increased level of circulating calcium. The parathyroid glands secrete parathyroid hormone (PTH) which serves to absorb Ca2+ from the intestines and the kidney’s tubules, and release Ca2+ from bone.
The thymus is located between the lungs (Figure 7.3) and plays a role in both the endocrine and lymphatic systems. Hormones released by the thymus include thymosin, thymopoietin and thymulin and are responsible for the development and/or regulation of T cells. Once T cells have fully matured in the thymus, they migrate to the lymph nodes where they help the body protect itself against autoimmunity and aids in fighting infection and disease. The thymus reaches its maxima size during puberty. After that, the thymus slowly shrinks and it replaced by fat. By 75 years of age, the thymus is essentially all fatty tissue.
The adrenal glands sit on top of the kidneys. (Figure 7.4) They have two distinct regions with two distinct functions. The outer layer is the adrenal cortex which surround the adrenal medulla. ACTH from the anterior pituitary triggers the adrenal cortex to produce steroidal hormones that fall into three classes: glucocorticoids, mineralocorticoids, and androgens.
The most abundant glucocorticoid is cortisol, which in addition to being triggered by ACTH also responds to CRH. Secretion of the most notable mineralocorticoid, aldosterone, is stimulated by a circulatory rise in potassium ions and a drop in sodium ions. Secretion of aldosterone also occurs in response to ACTH and angiotensin II, which is derived from the liver and then produced by the kidney. The adrenal cortex also produces DHEA which is a precursors to androgens such as testosterone and estrogen.
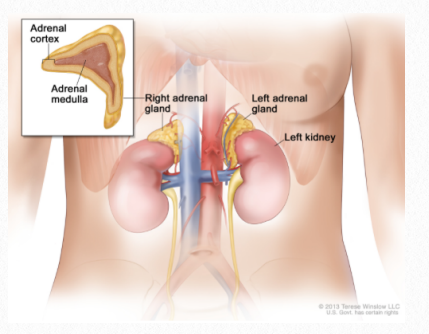
Figure 7.2 Adrenal glands
The adrenal medulla is part of the nervous system because it consists of masses of neurons that are part of the autonomic nervous system, specifically the sympathetic branch. However, it functions as an endocrine gland and releases epinephrine and norepinephrine. Both are released with physical and emotional stress.
Endocrine glands found in the pelvic region include the ovaries in females and the testes in men. Once mature, the ovaries produce steroidal hormones including a mixture of estrogens, of which estradiol is the most abundant, and progesterone. Synthesis and secretion of estrogen is stimulated by FSH which in turn is controlled by the hypothalamic GnRH. High levels of estrogen suppress GnRH providing a negative feedback loop. Progesterone production is stimulated by LH from the anterior lobe of the pituitary, which in turn is also controlled by GnHR and functions via a negative feedback loop.
The principle androgen, testosterone, is synthesized in the testes by the Leydig cells. Similar to progesterone, it is controlled by release of LH and participates in a negative feedback loop, such that a rising level of testosterone will suppress the release of GnRH from the hypothalamus.
Although estrogen is known as the female hormone, and testosterone the male hormone, the adrenal glands produce very low quantities of both hormones in both sexes. In addition, the ovaries release very small amounts of testosterone, while the testes release very small amounts of estrogen. See the appendix for details of the major endocrine glands, their hormones and actions.
Prenatal
The first endocrine gland to form in utero is the thyroid at approximately 3-4 weeks of gestational age. Prenatally thyroid hormones are essential for normal
maturation of the nervous system. Development of the pituitary occurs slightly later than the thyroid. Most of the pituitary hormones such as prolactin, LH and FSH are not secreted until adolescence or adulthood. However, ACTH, TSH, and GH are released in utero and begin to influence development. It is important to note that although GH plays a major role in growth and development during childhood and adolescence, it does not have the same effect on fetal growth (Carlson, 2009).
Infancy and Early Childhood
The endocrine system continues to develop during infancy and early childhood. The adrenal glands are particularly immature, with limitations in how the pituitary and adrenal cortex function together. This in part can account for the challenges toddlers with maintain homeostasis especially when the experience vomiting or diarrhea. Although GH did not have much of an effect on prenatal growth, it plays a tremendous role on cell proliferation and growth during infancy, childhood and adolescence. GH helps sustain a normal rate of protein synthesis and is especially important for cartilage production and overall bone development. Increased height during childhood is the most widely known effect of GH.

Figure 7.3 Children Playing
Adding to the effects of GH on bone development are the hormones released by the thyroid and parathyroids. T3, T4 and PTH are extremely important in the growth of bones and teeth as well as the brain and nervous system. When calcium levels are too low PTH will be released and calcium will be released from bones so that it’s available in the blood for nerve conduction. Infants born with hypothyroidism can have delayed motor and cognitive development (Sinclair & Dangerfield, 1998)
Late Childhood and Adolescence
During pre-puberty and adolescence, the endocrine system undergoes dramatic changes. Although the precise physiologic trigger for these changes is not thoroughly understood at this time, it is accepted that the hypothalamus initiates puberty through secretion of neuro-humeral releasing factors. These factors stimulate secretion of GH from the pituitary
which continues to promote protein synthesis and growth of the internal organs, muscle and bone. GH also allows for an increase in the use of fat metabolism for energy production and can help in improving endurance by assisting in maintaining glucose levels. Additionally, GH stimulates the liver to produce insulin-like growth factor -1 (IGF-1) a hormone that has growth-stimulating effects on a wide variety of tissues including stimulatory effects on osteoblast and chondrocyte activity to promote bone growth. It’s worthwhile to note that the largest and most predictable GH peak occurs about an hour after onset of sleep and that the amount of GH produced at night can represent 20-40% of the day’s total output (Sinclair & Dangerfield, 1998).

Figure 7.4 Adolescents
During adolescence, the hypothalamus also stimulates the thyroid by secreting TSH. The thyroid then releases T3 and T4 which help to regulate metabolism, energy, growth and nervous system activity. Thyroid hormone levels are especially elevated during the adolescent growth spurt.
Adolescence and puberty tend to be defined by sexual maturity and development of the ability to procreate. This is due to the hypothalamus’ production GnRH which stimulates the pituitary to release ACTH, LH, FSH. ACTH stimulates the adrenal cortex to release androgens which drive the dramatic changes in appearance that occurs during this time along with reproductive capabilities. LH and FSH work together to allow for normal functioning of the ovaries and testes. LH and FSH regulates testosterone release and sperm production, respectively in males. Whereas in females, LH and FSH regulate the release of estrogen and stimulates ovulation.
Adulthood and Older Adulthood
The earliest endocrine change that occurs after adolescence, is a reduction in GH. Although the degree of decline is quite variable across individuals it begins during the late 20s and affects both men and women. In men, it is estimated that GH levels are halved every seven years.
In later years, the term somatopause is sometimes used to refer to a transitional period of adulthood characterized by a decline or pause in the production of several important hormones, including GH. Beginning with the hypothalamus, there is a reduction of GHRH along with associated declines in the pituitary’s release of GH and the liver’s release of IGF-1. These declining hormones are associated with a variety of physiologic changes including a general reduction in protein synthesis; progressive reduction in lean body mass, which contributes to a decline in metabolic rate; increased deposition of adipose tissue, particularly abdominal fat; a reduction in bone mass and density; and a general decrease in immune function. Abdominal fat accumulation is linked to heart disease, high blood pressure and type 2 diabetes, which can occur in isolation or together in the form of metabolic syndrome. Reductions in bone mass and density increases the risk of osteoporosis and fractures (Knight & Nigam, 2017).
Also contributing to the gradual reduction in basal metabolism that occurs during middle and older adulthood is a reduction of TSH produced by the pituitary with a subsequent decline in serum levels of T3. Thyroid function testing is often recommended for adults with chronic conditions such as chronic obstructive pulmonary disease, hypertension, and diabetes because they tend to be associated with reductions in circulating thyroid hormones, particularly T3.
The parathyroid may contribute to the observation of declining bone density in later adulthood because as blood calcium levels fall, PTH is released, triggering calcium to be released from bone. Studies have shown that most people, as they get older, have significantly increased levels of circulating PTH (Braverman, 2009; Portale et al, 1997).
Changes in the hormones of the adrenal glands also occurs during middle and later adulthood. Although aging is associated with a decline in the secretion of epinephrine, plasma levels remain relatively constant as clearance by the kidneys is usually reduced. Aldosterone on the other hand, which regulates plasma levels of sodium and potassium and plays an important role in blood pressure control, decreases with age and appears to contribute to postural hypotension and the light-headedness that is experienced by older people when they stand up.
Research results of cortisol level changes with aging is contradictory. Initial studies suggested that there could be a 20-50% increase in the mean levels of cortisol secretion between the ages of 20 and 80 (Chahal and Drake, 2007). More recently, however, it has been shown that this is not necessarily true because in some people, cortisol secretion diminishes with age, while others have cortisol levels that remain relatively stable throughout life (Wolf, 2015). Nevertheless, there does appear to be a link between increased cortisol levels, reduced bone density and increased risk of fracture. There is also growing evidence that a higher cortisol concentration can contribute to the loss of cells from the hippocampus, resulting in hippocampal atrophy, which is often associated with a reduction in cognitive function in older people (Chahal and Drake, 2007). Other studies have shown that age-related increases in cortisol may also be linked to memory loss and sleep disorders (Chahal and Drake, 2007; Wolf et al, 2005).
The release of melatonin declines dramatically over time, largely due to calcification of the pineal gland such that 60-year-olds have 80% less melatonin in their blood compared to teenagers. Furthermore, commonly prescribed medications for older adults such as beta-blockers and non-steroidal anti-inflammatory drugs can reduce melatonin levels even
further. Decreased melatonin levels are linked to an increased prevalence of sleep disturbances which can have a negative effect on cognitive function and can exacerbate age-related changes in the brain.
Adulthood includes fertile years during which the testes and ovaries produce sperm and ova, respectively and through sexual intercourse, may fuse to form an embryo. In middle and old age, the reproductive system undergoes significant changes that result in a gradual decline in fertility and fluctuations in the production of sex hormones that can have far-reaching effects.
In females, it begins with a decline in estrogen production as the number of ovarian follicles begin to decline, especially between the ages of 40 – 50. This triggers menopause, which is a complete cessation of ova development even though the levels of FSH and LH can be initially high or unchanged. This period of time is called menopause and is often associated with hot flashes. This phenomenon appears to be related to an increased level of FSH and a decreased level of estrogen. Less estrogen also seems to affect serotonin levels in the hypothalamus, causing fluctuations in the set point of the thermoregulatory center (Santoro, et al, 2015).
Menopause is also associated with decline in connective tissue elasticity which can negatively affect the vagina, bladder, and urethra. This can lead to dyspareunia (uncomfortable or painful sexual intercourse), reduced libido and urinary incontinence. Breast tissue is also estrogen sensitive and therefore a reduction in estrogen can lead to a loss of supporting connective tissue in the breasts. In additions, a reduced level of estrogen can lead to a decreased in bone density.
Changes in the reproductive system and associated hormones also occurs in males. This is sometimes referred to as andropause, although there has been far less literature published on andropause when compared to menopause. Males will experience an age-related reduction in testicular mass with an associated reduction in testosterone and sperm production.
Unlike females who become infertile during menopause because ova cannot be produce, men can remain fertile through their 80s because sperm can still be produced. However, erectile dysfunction (ED) may present a problem due to compromised elasticity of connective tissues. In addition, a reduced testosterone level can cause the penis to shrink in both its flaccid and erect states. Furthermore, secretions from the seminal vesicles and prostate gland decreases with age so the volume of ejaculate is reduced (Knight & Nigam, 2017).
Final thoughts
Through its network of glands and hormones, the endocrine system plays a role in nearly aspect of development and aging. It drives growth during infancy and childhood, development of reproductive capabilities in adulthood, and multi-system changes and declines in older adulthood. Rehabilitation professionals can play an important role in educating patients and clients about the effects the endocrine system can have on function and health and should consider those effects when developing plans of care for people at different stages of life.
“If you skrew the endocrine system, you lose the
pathways to self. When endocrine patterns change,
it alters the way you think and feel. One shift in the
pattern tends to trip another.”
-Hilary Mantel
“Hormones are very powerful things. We are helpless in their wake.”
-Meg Cabot
References
Braverman, E.R. (2009). Age-related increases in parathyroid hormone may be antecedent to both osteoporosis and dementia. BMC Endocrine Disorder, 9, 21.
Carlson, B.M. Human Embryology and Developmental Biology, 4th edition, Philadelphia: Mosby Elsevier, 2009.
Chahal, H.S., & Drake, W.M. (2007.) The endocrine system and ageing. Journal of Pathology, 21(2),173-180.
Hiller-Sturmhöfel, S., & Bartke, A. (1998). The endocrine system: an overview. Alcohol Health and Research World, 22(3), 153–164.
Knight, J., Nigam, Y. (2017). Anatomy and physiology of ageing 7: the endocrine system. Nursing Times [online]; 113(8), 48-51.
Knight, J., Nigam, Y. (2017). Anatomy and physiology of ageing 8: the reproductive system. Nursing Times [online]; 113(9), 44-47.
Portale, A. A. , et al (1997). Aging alters calcium regulation of serum concentration of parathyroid hormone in healthy men. American Journal of Physiology, 272, 139-146.
Santoro, N., Epperson, C.N., & Mathews, S.B. (2015). Menopausal symptoms and their management. Endocrinology and Metabolism Clinics of North America,44(3), 497-515.
Sinclair, D., & Dangerfield, P. Human Growth After birth, 6th edition, New York: Oxford University Press., 1998.
Wolf, O.T., et al (2005). Subjective memory complaints in aging are associated with elevated cortisol levels. Neurobiology of Aging, 26(10), 1357-1363.
Images
Title page. [Image File]. Retrieved from https://www.hormone.org/what-is-endocrinology/the-endocrine-system
Figure 7.1 Hormones of the Hypothalamus, Thyroid, Pituitary and Pineal Gland. LadyofHats. Retrieved from https:// commons.wikimedia.org/wiki/File:Endocrine_central_nervous_en.svg
Figure 7.2 Adrenal Glands. Retrieved from https://www.cancer.gov/publications/dictionaries/cancer-terms/def/adrenalgland
Figure 7.3 Children Playing. United Nations Photo. Retrieved from https://wordpress.org/openverse/image/ 8c0e2060-7275-4861-b629-f1b7fddafe97
Figure 7.4 Adolescents. Photo by Gezelle Rivera. Retrieved from https://wordpress.org/openverse/image/ 63eccfd8-2450-481b-889c-459269ceaca9
Figure 7.5 Older Women. Photo by National Institute of Aging. Retrieved from https://wordpress.org/openverse/image/ee86c5b6-d946-4d2f-9257-1e6f1f5d951e
Figure 7.6 Older Man. Photo by Retrieved from https://wordpress.org/openverse/image/ff27009e-170a-47e6-967b319bb1e05dd9
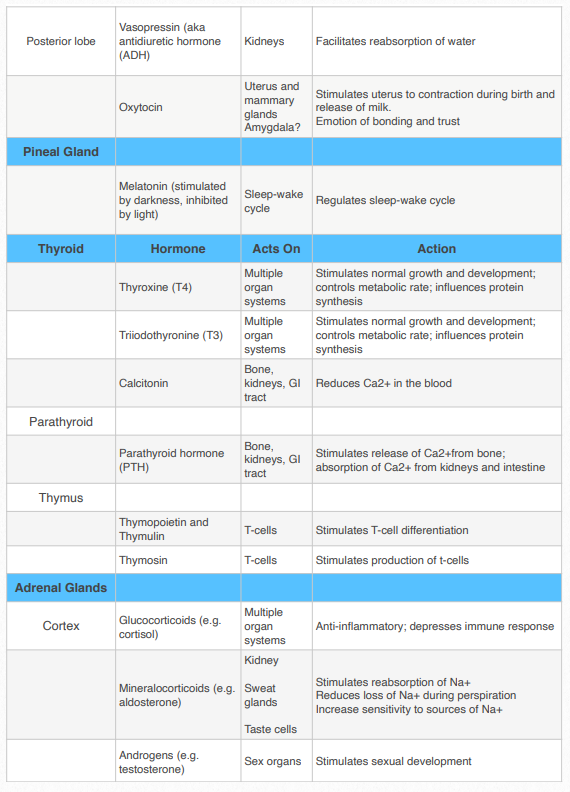
Appendix: Endocrine Glands, Hormones & Actions